Wound Sensors Trials Start: A Step Towards Reducing Diabetes-Induced Amputations
In The News | 27-05-2023 | By Robin Mitchell
Recently, researchers from the University of Nottingham have been awarded £900K to develop smart wound sensors that can be used to determine if a wound is healing or is infected, thereby reducing the damage done from secondary infections in patients suffering from diabetes. What challenges does diabetes present to the NHS, how will the researchers use electronics to determine if a wound is infected, and what impacts could such smart sensors have on health?
What challenges does diabetes present?
Diabetes is a condition where the body struggles to maintain correct blood sugar levels, and this difficulty results from the inability to produce the correct insulin levels. Two main varieties of diabetes exist, type 1, and type 2, with type 1 being generic and type 2 being induced via external factors (such as obesity). In either case, if the condition becomes too severe, then the use of insulin injections is required to help maintain healthy levels of blood sugar. Without insulin, those with diabetes can quickly become severely ill, including organ failure, coma, and death.
So, it goes without saying that keeping on top of personal health and ensuring the correct insulin levels is essential for those with diabetes, but there are numerous other conditions that those with diabetes can face, and they are not always obvious. One such challenge when suffering from diabetes is that nerve endings can be damaged, reducing the sensation in the extremities.
This is problematic as wounds that form on the bottom of feet may not be noticed, and this can lead to infections (such as sepsis). If not treated quickly, infections can spread into the tissue and rest of the body. To stop the spread of deep tissue infection, amputation is often the only course of treatment; otherwise, multiple organ failure can result, eventually leading to death.
Overall, those suffering from diabetes are not just required to keep on top of their insulin levels but also to carefully monitor their health for secondary effects that can lead to complications.
Researchers developing wound sensors to catch infections early
The financial burden of wound management on the NHS is substantial, with costs reaching £8.3 billion annually, accounting for more than 4% of the NHS budget. A significant portion of this expenditure, between £837 and £962 million, is attributed to diabetes-related foot ulcers. At present, the primary method of assessing healing rates is through regular wound redressing, a process that can inadvertently promote infection and disrupt healing progress, further straining NHS resources.
Recognising the challenges faced by those with diabetes, a team of researchers from the University of Nottingham have recently been awarded £900K in funding to develop a new wearable sensor that will be able to detect if a wound is healing or infected.
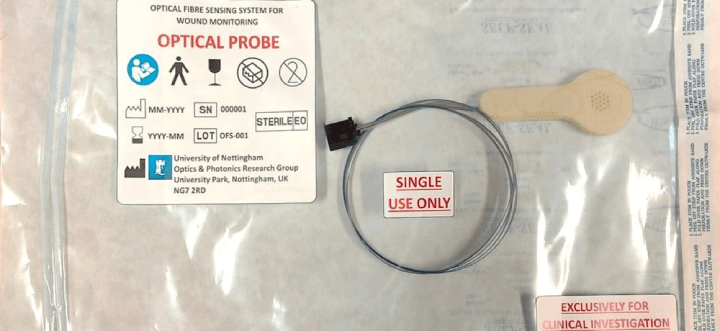
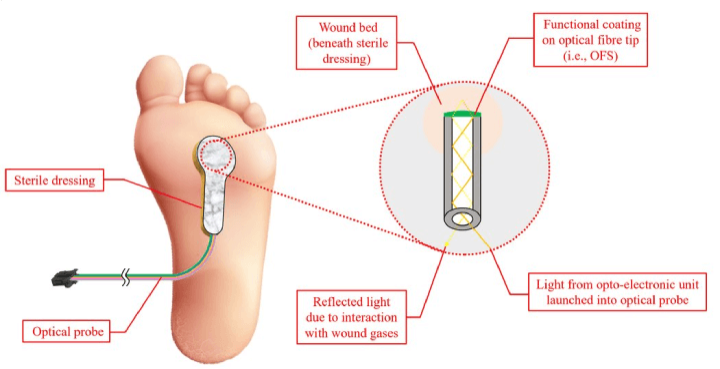
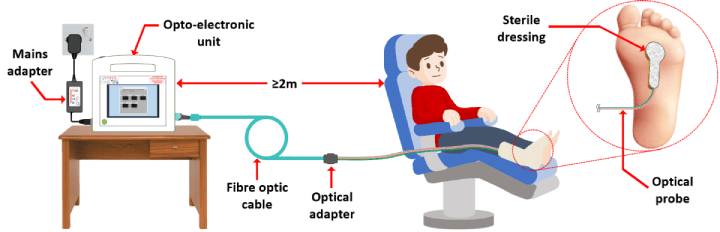
A prototype of the device has already been developed and is passed on an optic fibre that is inserted into a sterile bandage. Light shone down the fibre optic cable illuminates a wound, and reflected light comes back up the cable into a sensor. Wounds that are showing early signs of infection will have unique temperature, humidity, and gas signatures, and all of these can be determined via the fibre optic cable. If a wound that is not healing is detected, the use of immediate treatment methods such as cleaning and antibiotics can be provided, thereby eliminating any further complications.
The researchers are planning to test the sensor with ten diabetic patients suffering from foot ulcers over a period of 8 weeks in one-hour sessions every two weeks.
“Technologies to monitor wounds remotely and assess when things are going well or not so well, have the potential to have a significant impact on patients’ lives and health service costs. If we knew that a wound was healing well without having to use healthcare professionals time just to visually inspect it, it would make a huge difference to the NHS. Equally, knowing very quickly that wound healing had stalled, or an infection had developed would mean that we could commence appropriate treatments much more promptly, which would improve outcomes. I’m thrilled that the first trials of this device are being conducted at UHDB and that patients with diabetes will have the opportunity to support such ground-breaking research.” - Professor Fran Game, consultant diabetologist and clinical director of research and development at the Derby Clinical Trials Support Unit at University Hospitals of Derby and Burton NHS Foundation Trust.
If successful, this technology could significantly reduce the number of healthcare appointments required, thereby improving patient care and alleviating some of the economic burden on the NHS. For more detailed information about the cost of wound management to the NHS, you can access the full study here.
What impacts would such sensors have on the medical industry?
While the most obvious advantage of the newly developed sensor is the ability to reduce medical complications, there is an even bigger advantage; cost reduction. Generally speaking, medical complications are cheaper to fix the earlier they are addressed, which is why catching conditions early is so important (it also reduces the complexity of treatment and provides better outcomes).
In the case of wound management, it is believed that treating wounds costs the NHS in excess of £8.3 billion a year, or around 4% of the total budget. While not all of these will be related to diabetes, it is estimated that diabetic foot ulcers cost the NHS around £900 million each year. As such, if wounds can be better monitored and treated, this cost could be significantly lowered, even if the sensor used is expensive relative to traditional bandages. "These statistics are based on a study conducted by the BMJ Open and another study published in Diabetic Medicine. You can access the full studies here.
The use of such sensors also extends beyond those with diabetes; anyone with a wound that can potentially lead to complications can be monitored. For example, those who are in post-op care could use the bandage to ensure that no secondary infections are present.
Overall, what the researchers have developed only demonstrates the power of integrating modern electronics and technology into medical applications. Hopefully, this trial will pass with flying colours, and hospitals around the world start rolling out more intelligent systems to provide better healthcare.

