Plasmonic Biosensor for Detecting COVID-19
| 12-05-2020 | By Liam Critchley
While the world is trying to come grips with life under different normalities and social distancing policies, scientists are trying hard to find new ways of combatting the virus. By working on a vaccine to combat the spread of the disease or more effective testing and diagnostic methods that can tell if someone has, or has had, the coronavirus. While this coronavirus pandemic is the worst, it is the third coronavirus-based pandemic to hit the world, with the other two being the severe acute respiratory syndrome (SARS) outbreak in 2003 and the Middle East Respiratory Syndrome (MERS) in 2012. But the crucial part is that this outbreak already has more than 90 times the confirmed cases in those two outbreaks combined, so immediate solutions are needed to tackle it before it gets further out of hand.
Vaccines are a while off yet, so routine testing is vitally important at this stage of the pandemic and will continue to be so throughout the rest of the year. Even when the vaccine is available, people will still need to be tested, and it is one of the most significant solutions at the moment in the fight against the coronavirus. One issue with current testing methods is that they produce a high number of false-negative and false-positive results. Not ideal in the best of times, never mind when public health professionals and health systems are stretched beyond their standard capacity. So, while we currently have routine tests to diagnose if a person has/has had the coronavirus, new and more effective (i.e. more accurate) diagnostics are being sought after. There is a range of scientists in both academia and industry that are answering the call.
The Current Routine Method
While there are several different tests and diagnostic tools on the market—with more appearing all the time—the most common way (at the time of writing) of determining if someone has the coronavirus is the laboratory diagnosis method. This is known as reverse transcription polymerase chain reaction (RT-PCR). This method, while it is the current reference method, was the one that has been responsible for producing a large amount of false positive and false negative results, especially in the early days of the coronavirus outbreak.
RT-PCR is a laboratory technique that measures the specific RNA in a sample (i.e. the RNA pertaining to the SARS-CoV-2 virus). It is a mixture of reverse transcription of RNA into DNA and the amplification of specific DNA targets using a polymerase chain reaction. Measuring the amount of amplification in the sample by measuring its fluorescence determines the amount of RNA.
It has become a standard worldwide technique because the gene targets that are selected in different countries are genetically similar. This has made RT-PCR the most compatible technique around the world. But it is susceptible to nucleic acid contamination. Hence it can give false results. But, out of the many laboratory tests, it provides a much faster detection time. Nevertheless, there is a drive among the different adjoining industries—electronics, healthcare, nanotechnology, sensors, etc.—to create more efficient biosensors that can be used in clinical settings around the world.
A New Plasmonic Biosensor
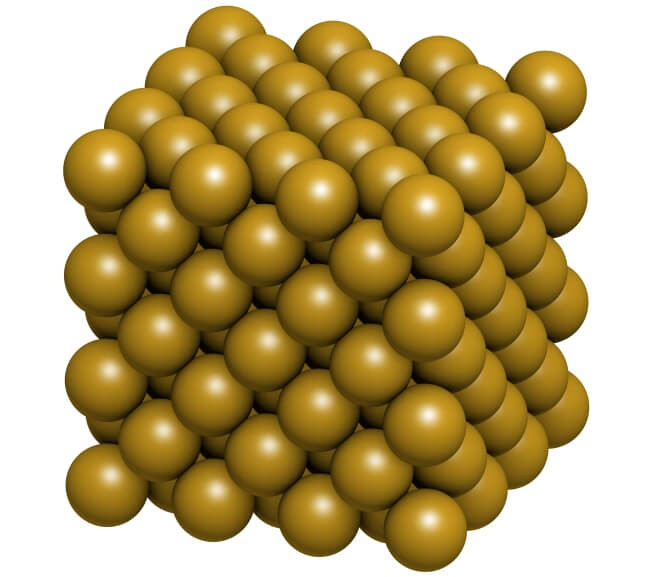
Research has emerged of a new type of biosensor that utilises plasmonic materials to enhance the sensitivity of the device. A plasmonic response is utilised in many kinds of sensors nowadays. It is when unreactive noble metals, such as gold, are utilised on the sensing surface to enhance the sensitivity of the device—typically by illuminating biomarkers because light interacts with the easily-excited free surface electrons of the gold atoms.
The plasmonic device developed by researchers in Switzerland works by utilising two different mechanisms—the plasmonic photothermal (PPT) effect and localised surface plasmon resonance (LSPR)—making it a dual-functional biosensor that has been designed to detect the SARS-CoV-2 viral strain.
The sensor itself utilises two-dimensional gold nanoislands as the active sensing material. To make it compatible with the SARS-CoV-2 virus, the gold nanoislands were functionalised with complementary DNA receptors to the vast single strands of RNA that are responsible for how the coronavirus functions.
The sensor works on a process of nucleic acid strand melting, otherwise known as nucleic acid hybridisation. This is when two complementary strands—i.e. the DNA receptors on the sensor and the RNA of the coronavirus—hybridise with each other. This typically happens at a point slightly below their melting temperature, so instead of melting, the strands hybridise together. A single mismatch between strands can significantly cause the melting temperature to decrease; thus, the strands don’t hybridise.
Light is shone on the sensing area by an LED light, and the changes in the hybridisation are picked up by an interferometric-based system. Because gold nanoparticles have large optical cross-sections, they absorb the light used in the sensing approach, and this helps to boost the sensitivity of the device. Upon absorption, the gold nanoislands generate thermoplasmonic heat which raises the hybridisation temperature in the sensing region. This higher temperature is what enables the nucleic acid hybridisation mechanism to occur accurately, and it enables the sensor to discriminate between two similar genetic sequences. This has allowed the sensor to be able to detect SARS-CoV-2 sequences down to the picomolar level and in multigene mixtures, making it a sensitive and reliable option for detecting if a patient has COVID-19.
The sensor being developed is just one of the many different types emerging out of academia and industry. While it is unknown if this specific sensor will be used on the frontline, it appears that new diagnostic methods need to come to the fore soon to prevent false positive and false negative results occurring. Moreover, the fact that the infection rate is significantly higher in this outbreak than previous outbreaks means that if there are any more outbreaks in the future, different types of sensors are going to be needed. So, even if these sensors do not make it to the frontline in the current outbreak, the research being performed now may help in producing the next generation of biosensors that could be used to tackle any future outbreaks.

