MIT's Wearable Ultrasound: New Era in Cancer Detection?
In The News | 18-08-2023 | By Robin Mitchell
Recently, researchers from MIT demonstrated a wearable ultrasonic imaging device capable of imaging breast tissue, raising hopes that breast cancer may be more easily detected by individuals at home. What challenges does breast cancer introduce, what did the researchers develop, and how do such devices demonstrate that the future of medical science is in individual wearables?
What challenges does breast cancer introduce?
Unlike many most common illnesses, which can be easily cured with the right drugs, cancer is a disease that introduces a whole range of various complications and challenges, whether it is limited life expectancy, inability for treatment, or whether it has spread to other areas in the body. While not all cancers can be treated, even if caught early, it cannot be understated the importance of regular check-ups and tests looking for the tell-tale signs of cancer.
In the case of breast cancer, if it is caught in the early stages, it has a 99% survival rate and is readily detectable via mammograms and physical inspection. However, if breast cancer is allowed to progress, the survivability rapidly drops, with stage 4 having a survival rate of less than 27%. Considering that examinations are relatively cheap and treatment options easily obtainable, dying from breast cancer in the 21st century can be particularly hard to deal with.
So, for a cancer that is easily detectable and treatable at the early stages, why do some women choose not to get screened? While every individual has their own set of reasons and circumstances for not attending check-ups, the most common reasons typically include being too busy, finding the examination painful and/or uncomfortable, and simply feeling that they are not at risk.
At the same time, doctors recommend that women self-check for lumps whenever they have time (such as in the shower), but this introduces its own set of issues. For one, it can be tricky distinguishing cancer from normal tissue, and this can get more complicated when trying to track and remember the size of specific lumps (this is also an issue when monitoring potentially cancerous moles).
With no at-home scanning systems of smart devices capable of detecting breast cancer with ease, breast cancer is able to creep up in those who least expect it.
MIT Researchers Create Wearable Ultrasonic Imager
Recognising the challenges faced with breast cancer detection, a team of researchers from MIT recently published their findings on a wearable ultrasonic device capable of imaging tissue under the skin.
According to the research paper published in Science Advances, the wearable ultrasonic imaging device developed by MIT researchers offers a non-invasive, painless, and cost-effective solution for early breast cancer detection. "The device's adaptability and precision make it a promising tool for self-examination, potentially revolutionising early detection methods," states the paper.
The system comprises two main parts; an adaptable cover with integrated magnets and an ultrasonic transducer that can be moved around. The adaptive cover is based on a honeycomb design that can flex and fit the natural shape of the breast, while numerous magnetic rings allow for the ultrasonic transducer to snap onto it. The sensor itself not only locks onto each of the magnetic rings placed around the flexible cover but can use the magnets to snap into different rotations of 60 degrees. As the sensor provides a singular 1D plane of view, the combination of the 6 different viewing angles and 6 different locations results in a complex ultrasound image comparable to those found in hospital systems.
Fig. 1. Design of the cUSBr-Patch
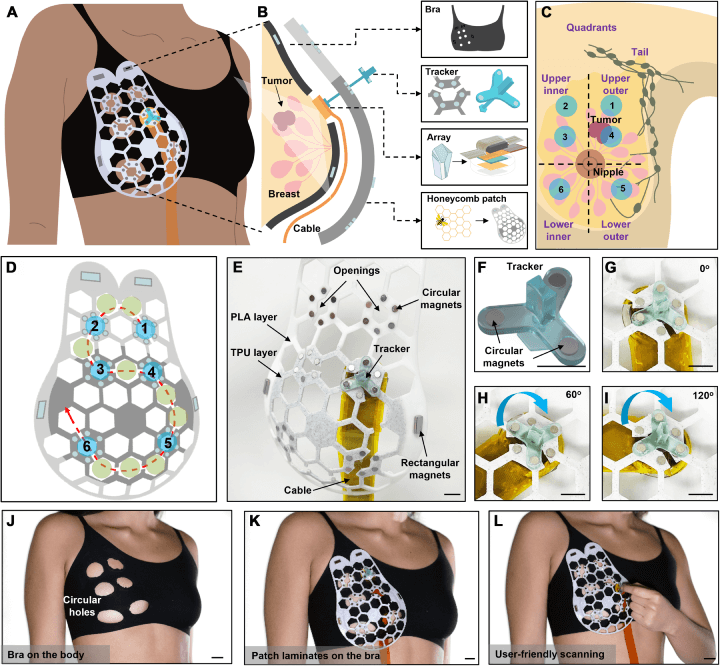
(A) cUSBr-Patch on the body. (B) Components: fabric bra, honeycomb patch, tracker, and 1D phased array. (C) Breast quadrants and patch alignment. (D) Honeycomb patch design with scanning trace. (E) Patch with array and tracker. (F) Tracker view. (G-I) Tracker's 360° rotation capability. (J) Bra with holes on a subject. (K) Patch on bra. (L) Scanning demonstration. Scale bars: 1 cm (E-I), 2 cm (J-L).
The system is able to detect features as small as 0.3cm up to 8cm into the tissue, providing patients with a significant ability to self-diagnose early stages of breast cancer. In a demonstration of the device, the researchers were able to see a small cyst in a 71-year-old patent who had a history of breast cancer.
Furthermore, the research paper highlights the device's capability to produce high-resolution images, making it easier to distinguish between benign and malignant tissues. This is crucial for accurate diagnosis and timely intervention.
Not only are there hopes that this device will reduce deaths relating to cancer, but it will also help to lower the barrier of entry to medical care. As many of the components are printed, it is believed that the cost of such a system will be significantly lower than that of systems currently in use in hospitals.
The expert opinion from Medical Design & Outsourcing also echoes the sentiment, stating, "This breakthrough technology from MIT has the potential to transform breast cancer screening, making it more accessible and less intimidating for women worldwide."
Why does this demonstrate the power of wearables in medical diagnosis?
If there is one fact that is undoubtedly true, it’s that wearables have so much power in the field of medical science, and they will likely become the dominant method of diagnosis in the future. As wearables are always worn, they can be used for constant monitoring of key vitals, generate tons of biodata, and then feed that data into AIs which can look for unusual patterns.
While the sensor developed by the MIT researchers wouldn’t be worn with everyday clothing, it may not be long before bras can be fitted with ultrasonic and thermal systems designed to actively monitor for subtle changes. If these changes can be identified early, it gives women the opportunity to find out if they have breast cancer at early stages. As such, it is possible to almost eliminate deaths from breast cancer in the future.
For now, the device developed by the researchers needs more development, but it clearly shows that the future of medical imaging doesn’t lie with large, expensive systems used in hospitals but with small devices found in the home.

