MIT Researchers Demonstrate Home RADAR for Monitoring Parkinson’s in Patients at Home
Insights | 04-10-2022 | By Robin Mitchell
Recently, researchers from MIT demonstrated a device that utilises RADAR to identify the gait speed of Parkinson’s patients capable of being used in homes. What challenges does monitoring of Parkinson’s present, what did the researchers develop, and how does this demonstrate the power of medical devices at home?
What challenges does monitoring Parkinson’s present?
When treating and caring for those with Parkinson’s, the severity of the condition must be well understood. At the same time, it is also important to recognise the rate at which the disease is worsening because this allows medical professionals to make informed decisions about courses of treatment and the eventual need for full-time care. But considering that current medical practitioners see patients on an infrequent basis, it can be very difficult to see the rate of degradation in an individual.
In the case of Parkinson’s, it is very easy for symptoms to go unnoticed for extended periods of time. For example, sight tremors in hands could be seen as being perfectly normal, and a worsening of these tremors may be difficult to spot. The same applies to gait (the posture and speed of walking); seeing changes in such patterns is very difficult to do.
One solution that has shown promise is the use of wearable devices to actively monitor patients, as data can be transmitted to a remote server and observed in real time by medical practitioners. However, current wearable devices are often bulky and uncomfortable, and this may cause distress in the patient being monitored. Furthermore, the patient must remember to put the device on after taking it off, which can be challenging for those with Parkinson’s.
MIT researchers demonstrate a RADAR device for monitoring gait
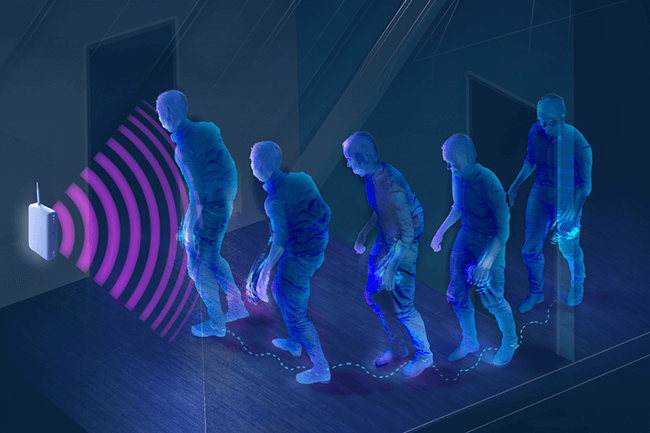
Recognising the challenges faced with wearable devices, researchers from MIT recently announced the development of a new device that can be installed in homes and used to monitor gait non-invasively without the need for any wearable devices.
The device utilises a type of RADAR that utilises low-power radio waves to map the area around them. The radio waves generated by the device are capable of passing through solid objects such as walls and chairs but reflect off humans due to the high water content. From there, the time of flight can be determined from bounced signals, and this results in a distance measurement. If multiple distance measurements are combined (as the person walks), it can be used to infer the speed of the person.
To test the validity of the device, 50 individuals were selected in a trial study, with 2/3 of the group having Parkinson’s with the other 1/3 being a control group, and the sensors were used to gather data over the course of a year. With the use of AI and eliminating outliers, the researchers were able to identify changes in speed caused by the progression of Parkinson’s. Furthermore, researchers were also able to identify the response of different medications through changes in speed, and this can be pivotal to helping doctors prescribe the best medications.
How does this device demonstrate the power of home medical devices?
The device developed by the MIT researchers demonstrates a growing trend in the medical technology market that is trying to bring medical monitoring to the home. The ability to monitor an individual’s health 24/7 allows for minute changes to be detected, and the introduction of AI into this field also adds the ability to identify issues before they become problematic.
But the introduction of medical technologies into the home also enables lower medical costs as preventative medical treatment is almost always cheaper than trying to treat conditions after they have progressed. Furthermore, the ability to integrate intelligence into medical monitoring through the use of AI also allows for every individual on the planet to have 24/7 access to a personal digital doctor that doesn’t require a waiting room, time off from work or being dismissed as a hypochondriac.
It is likely that the future of medical care will shift away from doctors and hospitals to the home hospital whereby technology drives diagnosis and treatment. Instead of needing to visit A&E for a cut that needs stitches, a robotic platform at home could provide the care required while an AI nurse observes the cut as it heals to identify potential infection. Only if expert intervention is needed will medical professionals be called in to provide additional treatment.

